Parkinson’s disease is a neurodegenerative disease that affects dopaminergic neurons in a brain area called the substantia nigra.

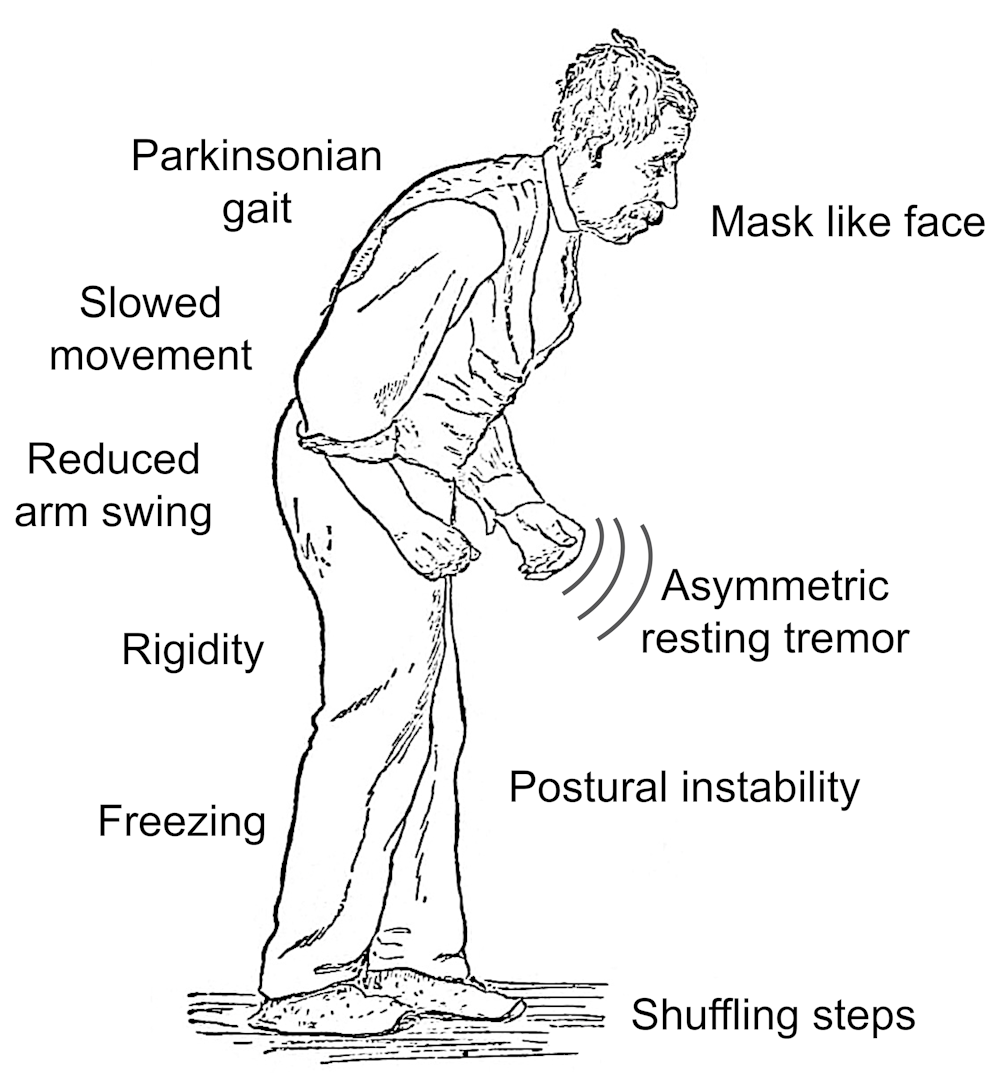
Your face expresses little or no expression in the early stage of PD.Your arms may not swing when you walk and your speech may confuse.PD symptoms get worse as time goes on.
Generally, symptoms develop slowly within years.Due to the diversity of the disease, the progression of symptoms is different in each patient.
SYMPTOMS
The symptoms may be different for everyone.The early stage symptoms may be slight and not become aware of.Symptoms start in one part of the body in general.
- Tremor : Tremor starts at your hand or fingers in general.Your hand may shake even your hand at rest.
- Bradykinesia: PD slows down your movement speed within time. Also, makes simple tasks difficult and making them time consuming.When you walking , your steps may be more short.Additionally, you drag your feet when you trying to walking.
- Stiff muscles : The muscle stiffness may be occur in your any part of body.Stiff muscles can be painful and limit your ROM.
- Poor posture and imbalance: Yor posture can bend over or balance problems may occur.
- Automatic loss of motion
- Speech change: Soft and rapid speaking can be seen. Your speech may be monotone.
- Writing changes: Typing can be difficult and your writing may seem small.
- Cramp (dystonia): sustained or repetitive twisting or tightening of the muscle.
- Drooling (sialorrhea): although not always seen as a motor symptom, excessive salivation or drooling can occur due to a reduction in normal automatic actions such as swallowing.
- Dyskinesia: involuntary, irregular writhing movements of the face, arms, legs, or trunk.
- Freeze: makes it look like it’s stuck in place, especially when starting a step, turning or navigating doorways. It’s a potentially serious problem as it can increase the risk of falling.
- Masked face (hypomimia): results from a combination of bradykinesia and stiffness.
- Soft speech (hypophonia): The soft, sometimes hoarse, voice that can occur in PD.
REASONS
Loss of neuron cells called the substantia nigra causes the PD. This situation decreases a chemical called the dopamine in the brain.Dopamine is vital for regulating body movements.Loss of dopamine is responsible of PD symptoms but the exact reason is unknown.The experts think that combination of genetic and environmental factors.

RISK FACTORS
- AGE: Young adults rarely get the disease.It usually begins in middle or late life and the risk increases with age. People usually develop the disease at age 60 or older.
- Heredity: Having a close relative with Parkinson’s disease increases your chances of developing the disease. However, your risks are still small if you don’t have many relatives with Parkinson’s disease in your family.
- Gender: Men are more likely to develop Parkinson’s disease than women.
- Exposure to toxins: Continuous exposure to herbicides and pesticides can slightly increase your risk of Parkinson’s disease.
TREATMENT
Parkinson’s disease cannot be cured, but medications can often help control your symptoms. In some later cases, surgery may be recommended. Your doctor may also recommend lifestyle changes, especially continued aerobic exercise. In some cases, physical therapy focusing on balance and stretching is also important. A speech-language pathologist can help improve your speech problems.
PHYSIOTHERAPY
Physical therapy cannot cure Parkinson’s disease because neurological damage cannot be reversed with physiotherapy. But therapy can help you compensate for the changes that the condition brings. Physiotherapy involves learning about new movement techniques, strategies and equipment. A physical therapist can teach you exercises to strengthen and relax muscles. Most of these exercises can be done at home. The goal of physical therapy is to improve your independence and quality of life by improving movement and function and relieving pain.
In addition to traditional physical therapy, basic exercises such as new technology virtual reality and robot-assisted training and complementary exercises such as Tai Chi, dance, Qigong and Yoga have provided awareness and benefit in motor development in Parkinson’s.
Walking training with signs : It has been suggested to use external rhythmic cues to support motor learning.[1] (Rochester et al., 2010) Musically marked gait training can facilitate more complex movements during challenging activities and improve pertubation and muscle strength.
Gait training using the treadmill: Many studies have examined the effects of walking on a treadmill, and the results for people with Parkinson’s are positive.
People with PD were trained to walk on the treadmill 2-3 sessions per week, and the training took 4-8 weeks.The positive effects of treadmill training on walking speed, stride length and walking endurance were reported.[3] (Ganesan et al., 2014; Picelli et al., 2013)
Brisk walking: The aim of walking in Parkinson’s disease is to increase the patient’s arm swing and trunk mobility. In addition, it helps to improve endurance and balance performance in elderly patients. In studies, the total number of daily steps increased in patients with Parkinson’s in a 6-week brisk walking program.[4] (Mak et al.,2016)
Nordic walking: They integrated northern walking into the 6 and 12-week program in individuals with Parkinson’s, as a result of which the walking speed and number of steps of the patients increased. The time spent on walking to and from the return time decreased. In other studies, it was observed that it reduced depression and fatigue. In summary, nordic walking increases walking speed in individuals with Parkinson’s, but longer in the disease. term usefulness is not clear.
Virtual Reality And Game-Exercise Based Rehabilitation: With the virtual reality system in 4-12 weeks, long-term effects on stride length and balance were achieved in the long term, and functional activities of daily life and cognitive functions were utilized.[5] (Shen & Mak, 2015),
Balance training: Findings from a meta-analysis review suggest that highly compelling balance training, which includes displacement of the body center of mass, reducing the size of CSF and upper extremity support, may have positive results on postural stability. [6] (Allen et al., 2011) In terms of motor performance, strength training and movement strategy training showed a longer-term improvement in motor score during spraying in the Unified Parkinson’s Disease Rating Scale (UPDRS) phase than in the control group. [7] (Morris et al., 2015)
Tai Chi: Typical balance exercises in TC are to transfer the weight from one leg to the other, stability exercises are done by changing the location of the body mass center, and postural exercises are done by turning in different directions. All this improves walking ability and strength of leg muscles. (Li et al., 2012).[8]
Therefore, balance, gait and functional mobility should be applied in patients with TC PD to fight the disease by improving the mental state. (Choi et al., 2013) [9]
Dance : Dance includes movements such as stepping, turning and spontaneous changes of direction, walking. Dancing regularly improves body coordination, postural control, walking and aerobic endurance.
Physical therapy can generally contribute to:
- Balance issues
- Lack of coordination
- Tiredness
- Ache
- Walk
- Inactivity
- Weakness
- Important note: Some physiotherapists may apply diathermy (the application of local heat produced by high-frequency electrical current) to relieve muscle aches and pains. This can be dangerous for patients with deep brain stimulators. Exercise has been proven to protect health and well-being in Parkinson’s. It has also been shown to play a large role in strength, endurance, flexibility, functional practice and balance, and focus
Physical activity, especially aerobic exercise, can slow motor skill degeneration and depression. It also improves the quality of life of Parkinson’s patients.[10]
In mild to moderate Parkinson’s patients, inspiratory muscle training is expected to increase inspiratory muscle strength by contributing to the improvement of lung functions, thoracic mobility, functional capacity and cardiac autonomic function.[11]
RESOURCES
1)Rochester, L., Baker, K., Hetherington, V., Jones, D., Willems, A. M., Kwakkel, G., et al. (2010). Evidence for motor learning in Parkinson’s disease: Acquisition, automaticity and retention of cued gait performance after training with external rhythmical cues. Brain
Research, 1319, 103–111.
2)McNeely, M. E., Duncan, R. P., & Earhart, G. M. (2015). A comparison of dance interventions in people with Parkinson disease and older adults. Maturitas, 81(1), 10–16. https://doi.org/10.1016/j.maturitas.2015.02.007.
3)Ganesan, M., Sathyaprabha, T. N., Gupta, A., & Pal, P. K. (2014). Effect of partial weight-supported treadmill gait training on balance in patients with Parkinson disease. PM & R: The Journal of Injury, Function, and Rehabilitation, 6(1), 22–33.
4)Mak, M., Chan, W., Auyeung, M., Chan, A., Cheung, N., & Mok, V. (2016). Effects of a
home-based brisk walking program in improving activity volume and walking capacity
in people with Parkinson’s disease [abstract]. In Fourth World Parkinson Congress, Portland.
5)Shen, X., & Mak, M. K. (2015). Technology-assisted balance and gait training reduces falls in patients with Parkinson’s disease: A randomized controlled trial with 12-month follow-up. Neurorehabilitation and Neural Repair, 29(2), 103–111. https://doi.org/
10.1177/1545968314537559.
6)Allen, N. E., Sherrington, C., Paul, S. S., & Canning, C. G. (2011). Balance and falls in Parkinson’s disease: A meta-analysis of the effect of exercise and motor training. Movement Disorders, 26(9), 1605–1615.
7)Morris, M. E., Menz, H. B., McGinley, J. L., Watts, J. J., Huxham, F. E., Murphy, A. T., et al.
(2015). A randomized controlled trial to reduce falls in people with Parkinson’s disease. Neurorehabilitation and Neural Repair, 29(8), 777–785. https://doi.org/10.1177/1545968314565511.
8)Li, F., Harmer, P., Liu, Y., Eckstrom, E., Fitzgerald, K., Stock, R., et al. (2014).
A randomized controlled trial of patient-reported outcomes with Tai Chi exercise in Parkinson’s disease. Movement Disorders, 29(4), 539–545
9)Choi, H. J., Garber, C. E., Jun, T. W., Jin, Y. S., Chung, S. J., & Kang, H. J. (2013). Therapeutic
effects of Tai chi in patients with Parkinson’s disease. ISRN Neurology, 2013, 1–7.
Article ID 548240.
10 Wu, P.L., Lee, M., & Huang, T.T. (2017). Effectiveness of physical activity on patients with depression and Parkinson’s: a systematic review. PloS one, 12(7), eo181515
11) Montero Ferro A, P. Basso‐Vanelli R, Moreira Mello RL, Sanches Garcia‐Araujo A, Gonçalves Mendes R, Costa D, Gianlorenço AC. Effects of inspiratory muscle training on respiratory muscle strength, lung function, functional capacity and cardiac autonomic function in Parkinson’s disease: Randomized controlled clinical trial protocol. Physiotherapy Research International. 2019 May 14:e1777.

Leave a Reply