The group defined as”risky infant” is a group of infants who are frequently encountered by healthcare professionals working in the field of pediatrics and whose developmental retardation is observed due to various reasons. Early rehabilitation programs should be initiated as soon as risky babies are born. Early neuromotor evaluations have an important place in reaching the early physiotherapy applications and various interventions that risky infants need. Early period physiotherapy includes physiotherapy approaches that start in the neonatal period and last up to 12 months, some of which are indicated as 24 months in some sources and up to 36 months in others. The first years of the baby’s life are critical in brain development. Current studies predict that there is high renewal and rapid learning in the brain during infancy, and the intervention applied in this process may be more effective. Therefore, early identification of risky infants and appropriate interventions are of great importance.

RISKY INFANT
The group defined as “Risky infant” has a biological and environmental factor history depending on gestational age or birth weight, and these factors can lead to mortality and morbidity risk -especially neuromotor development retardation.
Risky babies should be monitored by healthcare professionals. Premature births in high-risk infants constitute 70% of neonatal deaths and 75% of neonatal morbidity.The risks of infant may cause some complications over time. These complications can be summarized as follows:
Neurological complications: Cerebral palsy, epilepsy, hydrocephalus, etc.
Pulmonary complications: Pneumonia, chronic lung disease, respiratory distress syndrome, etc.
Cognitive complications: Mental retardation, attention deficit hyperactivity disorder, learning problems, memory-concentration and coordination problems, behavioral problems, etc.
Sensory complications: Visual, hearing, speech problems

CAUSES INFANTS TO BE INCLUDED IN THE RISKY BABY GROUP
*Premature births (especially infants under 1500 grams and before 32 weeks): While on-time birth covers 37-41 weeks, the birth of the baby below 37 weeks is called premature.
*Low birth weight: If the baby’s birth weight is in the range of 2500-3999 gr, it is called normal birth weight, and if it is below 2500 gr, it is called low birth weight.
*Perinatal asphyxia: Failure to provide placental or postpartum pulmonary gas exchange is a condition seen with biochemical changes such as hypoxia, hypercapnia and acidosis
*Hypoxic ischemic encephalopathy: It is the most severe form of perinatal asphyxia, intrapartum hypoxia or acute progressive encephalopathy caused by late antepartum cerebral ischemia and hypoxia.
*Intraventricular bleeding: It occurs due to the intrinsic weakness of the germinal matrix vein and fluctuations in cerebral blood flow. It causes the development of many neurological sequelae.
*Periventricular leukomalacia: PVL is the hypoxic-ischemic necrosis of the white matter, especially in the dorsal and lateral sides of the lateral ventricles.
*Muscle tone disorders (hypotonia, hioertonia, dystonia)
*Hyperbilirubinemia: Elevated bilirubin levels. It is also called neonatal jaundice.
*Respiratory distress syndrome: Pulmonary insufficiency due to structurally immature lung and sulfate deficiency.
*Viral infections: Intrauterine infections not only affect the immature brain, but can also cause secondary neural damage after cerebral ischemia. Chronic exposure to microorganisms such as cytomegalovirus, herpes simplex virus, toxoplasmosis, rubella, group B streptococcus may cause intrauterine inflammation and fetal brain damage.
*Fetal alcohol syndrome
* Presence of recurrent seizures
* Presence of neurological problems due to congenital causes
*Hydrocephalus/microcephaly *Peripheral nerve lesions (Brachial plexus)
*Musculoskeletal system abnormalities (Torticollis, arthrogryposis)
*Myelodysplasia (Spina bifida)
*Intrauterine developmental retardation
*Neonatal drug withdrawal syndrome
* Infants with chromosomal anomalies affecting development

HIGH-RISK INFANTS
– born less than 32 weeks of gestation and under 1500 g
– Major morbidity conditions such as bronchopulmonary dysplasia, cystic periventricular leukomalacia and intraventricular hemorrhage (stages 3 and 4), hydrocephalus
– Surgical conditions such as APGAR score of less than 3 or 3per minute in the fifth minute
– Seizures
– Shocks requiring inotropic/vasopressor support
– Infants born to HIV-positive mothers
– Neonatal bilirubin encephalopathy (kernicterus)
– Twin to twin transfusion
– Stage 3 hypoxic ischemic encephalopathy
– Surgical conditions such as diaphragmatic hernia or tracheosophageal fistula
– Small for Gestational Age, SGA,LESS than 3 percentile, or large for gestational age (Large for Gestational Age, LGA, greater than 97 percentile)
– Receiving mechanical ventilation for more than 24 hours
– Inner and prolongedhypoglycemia and hypocalcaemia
INFANTS WITH MODERATE RISK
– babies born in the december of 33-36 gestation week, 1500-2500 g
– Twins and triplets
– Neonatal sepsis
– Stage 2 intraventricular hemorrhage
– Babies with sepsis clinically and on imaging
– Stage 2 hypoxic ischemic encephalopathy
– Hypoglycemia (blood sugar <25m/dl)
LOW-RISK BABIES
– babies born at 37 weeks of gestation and above and around 2500 g
– Suspected sepsis
– Transient hypoglycemia
– Stage 1 hypoxic ischemic encephalopathy
– Intraventricular hemorrhage of preterm stages 1 and 2, in which no abnormalities were observed after the fortieth week of gestation

EVALUATION OF INFANTS AT RISK
Turkey, the survival rate of risky infants increases due to the development of neonatal care services in the last 20 years, however, the rate of problems that may affect the later periods of life in these infants also increases.
The first step in the early rehabilitation program is evaluation. Neuromotor evaluations are used for many purposes in infants at risk. Neuromotor evaluation of the child is generally examined under the headings of motor, sensory, personal, social and language development. The purpose of using neurodevelopmental and neuromotor evaluations is to evaluate the relationship between motor, neurological and behavioral functions, to distinguish between typically developing infants and those affected by the motor, to determine developmental retardation or if there is any problem (presence of central nervous system lesion, etc.) in the early period, to predict the problems and consequences that may occur in the future based on current performance, to analyze the changes that occur over time with the effect of treatment and environmental factors, to monitor the progress of development and to determine the effect of early interventions.
In risky babies, the evaluation is made in a bright, comfortable, quiet, warm or cold room, while the baby is dressed as little as possible, calm and with his/her family. It is preferable to do it about 2 hours after feeding.
WHAT ARE THE NEUROMOTOR EVALUATION METHODS USED BY PHYSIOTHERAPISTS?
OBSERVATION
One of the most important components of the physiotherapist’s evaluation is the observation of movement. The evaluation of cognitive, sensory, emotional, and social aspects of the motor movements of infants as a whole can provide the identification of infants in need of early rehabilitation.
EVALUATION OF MUSCLE TONE
Passive tone is the resistance of the extremities to passive movement. Active tone is tested by observing static posture, automatic reactions, spontaneous movements and reflex tests.
If the baby has hypertonus;
– When the baby is brought to an upright position, the neck goes to hyperextension and the legs go to extension.
-Spontaneous movements are difficult to do.
– If the tonus increase is in the extremity muscles, the movements of the head and body become difficult.
– The body is asymmetrical.
– There are pathological reflexes.
-Primitive reflexes may increase in severity.
If the baby has hypotonia;
-The extremities are usually in extension and abduction.
-Spontaneous movements have decreased.
-Midline orientation and flexor patterns are scarce.
– The flexor and extensor muscles of the neck are weak.
-Outpatient dorsi flexion and wrist flexion movement limit have increased.
– Wide joint movement and flexibility are dominant in hip, knee and shoulder and elbow joints.
– The severity of hypotonin is related to gestational age.
Evaluation of Reflex Development
Evalution of reflex development helps early diagnosis as well as determining a possible disease and the severity of the disease. In the normal development of infants, primitive reflexes (spinal and brainstem reflexes) gradually disappear and are replaced by correction and equilibrium reactions. However, if the inhibition control of high centers is delayed or impaired, primitive patterns gain superiority. These types of lesions prevent the inhibition of primitive reflexes.

Reflexes that need to be evaluated during the early rehabilitation process are as follows:
Moro Reflex: Gestational should start at 32 weeks and disappear around 5-6 months. When a stimulus such as a sudden sound is given when the baby is in the supine position, moving the floor on which s/he is lying, or gently lifting and releasing the hands, it is expected that extension in the body, abduction and extension in the upper extremities, and adduction and flexion will follow.
Babinski Reflex: Expected to disappear around 12 months. When the base skin is drawn from the outer side of the base towards the middle metatarso-phalangeal joint with a blunt object, it is expected that the thumb will come to the dorsiflexion instead of the plantar flexion response of the fingers that should normally be seen.
Search/Suction Reflex: It is seen in the first 3 months after birth. It is the search reflex that the baby turns his/her head to that side with the warning applied to the edge of the mouth. Suction reflex is the initiation of suction movement by touching the lips or inserting an object into the mouth.
Palmar and Plantar Comprehension Reflex: It starts in the gestational 32nd week and is replaced by voluntarycapture movement for 3-5 months. When the physiotherapist contacts the palm of the baby with his/her own finger from the ulnar edge, the baby’s fingers are expected to close and catch (palmar grip). When the toes are touched close to the starting point of the toes at the foot of the baby, it is expected that the toes will pass into flexion and catch the touching finger (plantar capture).

Flexor Withdrawal and Extensor Repulsion Reflex:(2.)- The baby lies on his back, the head is in the middle position and the extremities are in extension. The limb stimulated by the stimulation given to the plantar face of a foot is expected to go to flexion (flexor pull). The baby lies on his back, the head in the middle position, one leg in the flexion and the other in the extension position. With the stimulation given to the plantar surface of the extremity in flexion, that extremity is expected to go to extension (extremity pushing).
Step Taking and Automatic Walking Reflex: It is seen in the first 6-8 weeks of life. The baby is held and lifted from the armpits, and when the soles of the feet touch the examination table, it is expected that successive flexion-extension movements similar to stepping on the legs will occur.
Neck Correction Reaction: (4.8.months)- It’s most pronounced in the eighth month. With maturation, the tonic neck reflex turns into a neck correction reaction. When the head is turned to one side, it is expected that the body and extremities will automatically turn to that side and the rolling movement will develop.
Asymmetric Tonic Neck Reflex: It starts at the 35th week of gestation and disappears around 3-4 months. The baby is reclined in the supine position. The head is rotated 90 degrees to the right or left from the midline. In the meantime, it is expected that extension in the arm and leg on the ipsilateral side of the dizziness and flexion in the opposite arm and leg will occur.
Tonic Labyrinth Reflex: It decreases within the first 6 weeks and disappears within the first 3 months. Makes the body stand upright against gravity. In the child lying face down, the feet should be in flexion and under the abdomen, the arms should be in flexion and at chest level.
Galant Reflex: It continues until the second month. Both sides need to be examined, asymmetry is pathological. The baby is kept supported in the prone or ventral position, and a slight pressure is applied from the edge of the spine to the last rib and iliac region by keeping the index finger parallel. It is expected that the baby will bring the body to lateral flexion towards the given warning side.
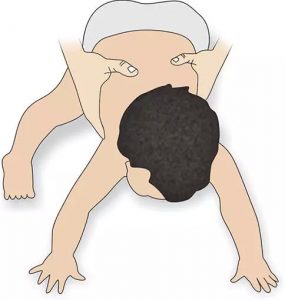
Protective Extension Reflex (Parachute Reaction):It starts at the sixth month and lasts a lifetime. When the child is held from the ankles or pelvis and brought closer to the ground in the upside-down position, it is expected that the arms will suddenly extend to protect the head, and that extension and abduction will occur in the fingers.
MOTOR EVALUATION Standard tests are the most commonly used tests in evaluation. Standard tests compare the performance of the baby according to the test content, not the population, and provide an indicator of independent performance. These tests generally investigate the distinction between normal and abnormal development. Evaluations are varied; some of them evaluate the baby’s spontaneous movements and antigravity postures, some of them require touching the baby to reveal movement, and some of them reveal social/psychological/behavioral evaluation.
–Alberta Infant Motor Scale (AIMS): Can be used up to the walking child (0-18 months) independent of thenewborn baby. It allows the family and clinician to learn about the child’s motor status and to measure motor performance development before and after treatment. It is observed that the child performs spontaneous motor behaviors with a certain postural control. It measures weight transfer, posture and antigravity movements in supine, prone, sitting and standing positions with 58 items. It is a reliable test with norm reference. It takes 10-20 minutes to apply.
-The Neurosensory Motor Assessment Questionnaire (NSMDA) is used to evaluate infants or children aged 1 month to 6 years. It is used to characterize the progressive motor development in long-term follow-up of premature children, to identify special problem areas in motor development, to assist in the diagnosis of CP, to compare motor results in different problems, and to predict the motor development and cognitive performance of premature children. The test shows whether the motor development and movement components of infants and children are within normal limits, suspicious or abnormal. The parameters of this criterion-referenced test are age-appropriate motor abilities, tonus, deep tendon reflexes, movement patterns, postural reactions and balance, tactile, proprioceptive, visual and vestibular sensory systems.
–Hammersmith Infant Neurological Examination (HINE) is used to evaluate infants up to24 weeks of age. The aim of the study is to determine the higher risk of neurological anomalies in preterm and on-time babies at other stages of their lives. HINE is a preventive battery in terms of early identification of neural disorders. It includes tonus, reflexes, abnormal signs and movements, cranial nerve functions, posture, movement, orientation/behavior evaluations, and is norm-referenced.
–Bayley-III Infant and Child Development Rating Scale (Bayley III) was developed by Nancy Bayley. It was renewed in 1993 and Bayley Infant and Child Development AssessmentScale-2. (Bayley-II) version has been published. Bayley-II is used to evaluate children aged 1-42 months in the USA and to monitor their development. In general, it evaluates the developmental status of the child in accordance with special ages.
-The Test of Infant Motor Development (TIMP) is a test used to measure babies up to 4 months of age, including premature babies born at32 weeks of age. It consists of 31 items in standard format with 28 items scored as “passed/left” by observing spontaneous activities. It performs measurements in the fields of stabilization of the head in various positions, organizing the body according to the position, distal selective control of the finger-wrist-wrist-ankle, antigravity control of arm and leg movements. Its application lasts between 25-45 minutes. It is a reliable test with norm reference.

–Prechtl‘s Assessment of General Movements (GMs) is a criterion-referenced test that examines the spontaneous movements of theprenatal baby, the newborn and the adjusted infant up to 5 months of age. The evaluation includes the classification of observations and spontaneous movements in the supine position. It is said to be effective in revealing conclusions about neurological disorders such as SP around the age of 2.
-Dubowitz Neurological Assessment is based on the traditional, neuromaturative side of
development. It is frequently used in neonatal clinics. It examines whether the preterm and timely newborn baby has a neurological problem in the neonatal period or immediately after birth, or whether it tends to have a neurological problem. It consists of 32 items including 4 areas: reduced response to repetitive stimulation, movement and tonus reflexes and behavior. It is a valid and norm-referenced test.
–Infant Motor Profile (IMP) is based on video analysis of spontaneous movements of infants between3-18 months. With the 15-minute video analysis, the baby’s supine, prone, sitting, standing, lying down and grasping movements are evaluated. It is evaluated not only whether the baby succeeds or not, but also how the baby succeeds. With 80 items, 5 areas of movements are evaluated: diversity, ability to choose, symmetry, fluidity, performance. It is a valid and reliable test with norm reference.
-Movement Assessment of Infants (Mai) aims to determine the change in motor dysfunction and motor dysfunction of infants up to 1 year of age from birth and to create a treatment program. It is a 65-item criterion referenced tool for evaluating 4 areas. These areas are: muscle tone, reflexes, automatic reactions and voluntary movements. Each item is scored between 0-4 or 0-6. It measures the quality and competence level of spontaneous movements such as basic posture and behavioral movements initiated by the child in the developmental curve.
-The Peabody Developmental Motor Scales-2 (PDMS-2) is used in children aged0-5 years. It evaluates the coarse and fine motor. The gross motor scale evaluates reflexes, balance, and activities with and without locomotors. The fine motor scale evaluates grip, hand functions, hand-eye coordination and hand skills. The application time lasts 45-60 minutes. It is a reliable test with norm reference.
-The Harris Infant Neuromotor Test (HINT) evaluates motor and cognitive developmental disorders. It evaluates babies aged 2.5-12.5 months in 4 main areas: general information, caregiver’s thoughts, 21-item test section, general observation of the clinician. The application time is 15-30 minutes. It is a valid and reliable test with norm reference.
–Milani-Comparetti Motor Development Screening Test performs the motor evaluation where functional motor capabilities are associated with reflex structures. The person conducting the test physically manipulates the child to create a specific motor response. The expected reflex or reaction is recorded as “present or absent”. The application time is 4-8 minutes. It is a reliable test.

SENSORY EVALUATION
Tactile, proprioception, vision, hearing senses should be evaluated in the sensory evaluation ofrisky infants. Crying in the baby should also be evaluated. The baby may not cry, continuous or excessive crying may be seen.
PHYSIOTHERAPY AND REHABILITATION PROGRAMS APPLIED WITHIN THE SCOPE OF EARLY INTERVENTION IN RISKY INFANTS
Early neuromotor evaluations allow risky infants who need early physiotherapy and intervention to reach them. Early rehabilitation programs in high-risk infants should start as soon as they are born. Early physiotherapy includes physiotherapy approaches starting in the neonatal period and applied up to 12 months (24 in some sources, 36 in some sources). The first year of the baby’s life is critical for brain development. It is important to identify infants with developmental retardation in the early period and to be able to perform appropriate interventions, because recent studies have suggested that intervention during infancy may be more effective when there is high brain regeneration and rapid learning. Early intervention applications provide follow-up of high-risk infants even if they cannot change the physical outcome such as Cerebral Palsy in infants with neurodevelopmental disorders, cause a decrease in secondary musculoskeletal disorders and increase the functional abilities of children who will be diagnosed with Cerebral Palsy in the future.
Physiotherapy and rehabilitation applications are started in neonatal wards in the neonatal period and then continue in hospitals, homes and physiotherapy centers. Physiotherapy and rehabilitation approaches basically aim to gain normal functional movements and give normal sensory input by using the ability to learn quickly due to brain plasticity, to reach the most independent level possible physically, cognitively, psychologically and socially within the physiological and anatomical inadequacies and environmental limitations of the child.
There are many early-stage physiotherapy and rehabilitation intervention options that focus on the progression and normalization of motor development. However, no clear conclusion has yet been reached as to which method is more successful.

NEURODEVELOPMENTAL THERAPY APPROACH (BOBATH)
One of the most commonly used methods among early physiotherapy approaches in our country and in the world is the Bobath Neurodevelopmental Therapy Approach (NGT). Physiotherapists try to find a solution to the child’s motor disorder by stimulating normal development in this approach.
Today, it is at the forefront to provide active-dynamic treatment and functionality in the NGT approach. It is aimed to operate different intertwined activities in a movement flow in order to improve the balance and coordinate the movement. Posture impressive patterns are used instead of tonus regulation. It is tried to improve movement and posture control in different positions by planning according to the personal development of the child. The basic understanding of today’s Bobath approach is to activate movement in function and to maintain practices in daily life. Neurodevelopmental treatment approach focuses on motor learning principles and aims to improve the postural control of the child by using family-oriented approaches, functional education, restrictive movement treatment, strengthening, orthoses, BNT application, assistive tools and bimanuel education along with body straightness.

A.Approaches to NGT in the neonatal period
Positioning
It has an important place intreatment in order to regulatemuscle tone, to facilitate spontaneous movements, to ensure posture smoothness, to prevent muscle and skeletal deformations, to minimize respiratory and nutritional problems, to increase sensory input, to facilitate observation and intervention.

a) Backstroke Positioning: Ease of intervention, ease of observation, preference in umbilical catheter applications.
b) Face-down Positioning: It is the starting position for weight transfer and weight bearing. Activates head correction reactions, prevents craniofacial deformations, facilitates flexor response and neutral flexion posture, facilitates weight transfer around the hip and shoulder, prevents hyperextension of the neck and body, easier oxygenation, less energy expenditure, useful for development of shoulder movements, cranial shaping and hip position. However, care should be taken for sudden infant death syndrome!
c) Sideways Positioning: Facilitates rotation of the shoulder and pelvic girdle, increases coordination between the flexor and extensor group muscles, allows rotation in the opposite direction, facilitates flexor muscle development, increases midline orientation, increases awareness and sensory input of the shoulder and pelvic girdle, increases right and left side awareness, makes it easier to notice the lower extremities. It is the starting position for hand-eye coordination and extending the baby to an object. Since gravity has the least effect, midline activities of the upper extremity are stimulated and scapular mobility is provided.

Touch
Massage and light stroking are important in terms of increasing sensory input. Even if they are in the mechanical ventilator, the oral area should be stimulated in babies. Temporomandibular joint can be applied from the mouth. Deep pressure can be used on the upper lip. Hypersensitivity to touch in infants -especially in the oral area, palms and soles of the feet – can be seen. It is appropriate to give a deep warning. Rhythmic tactile stimuli are also effective. Mild rhythmic shaking, touching the face and body, and holding it in a vertical position may be recommended in infants with lateral and quick irritation.

Supporting Motor Development
Activities that the baby can and cannot do should be determined in a natural environment. Basically, the movements that need to be addressed are symmetrical supine and prone posture, head control, rotation, movements of arms and hands, prone forearms and standing on hands, sitting, crawling, sorting and walking. Normal tonus revealing movements and dynamic activities should be targeted. The main goal is to acquire normal “sensory-motor” movement patterns with continuous repetition of movements. Family education, information and participation in the active physiotherapy program are important for success.

B. NGT Approaches After Neonatal Period
1-Facilitations:It allows the child to perceive his/her body. The goal is to facilitate the harmonious movement of muscles and joints within functional movement.
2-Stimulation:
Proprioceptive stimulation, vibration, tactile stimulation (touch), vestibular stimulation, stimulation of the baby through sound are provided. The purpose of stimulation is to teach movement, to provide stabilization, to regulate tone, to gain the child’s own movement control while moving.
3-Communication:
It covers all communication ways with the family and the child. During therapy, the physiotherapist should wait for the child to do the movement and remain calm. The physiotherapist’s tone of voice is important. Propripeptive education should be given importance. Environmental factors affect the child’s functional capacity. These factors should be determined and rearranged according to the child. Hypertonic children should be spoken loudly for the purpose of stimulation in hypotonic children, what kind of things the dyskinetic child is afraid of should be determined and caution should be exercised. The family should be properly informed and encouraged to play a greater role in the care of the child. The active participation of the family in the implementation program is important and should be encouraged. Family training is important for the correct application of positioning and holding techniques. With the help of the family, these techniques should be adapted to daily activities. The family should understand the objectives of these positions and should also be taught appropriate transport techniques.

Sensory Integration Therapy
It was developed by Jean Ayres to decipher the relationship between behaviors and the nervous system. the 5 basic hypotheses are as follows:
-The potential for changes in the brain that develops throughout life is called neuroplasticity.
-A strong relationship between the cortical and subcortical structures of the brain is necessary for proper sensory decency.
-Sensory integrity functions follow a natural developmental sequence.
-Depending on the environmental conditions, appropriate sensory responses are revealed.
-The development of sensory integrity can be facilitated.
According to Jean Ayres, sensory integration therapy should be designed in the form of games to enable and improve the child’s learning. Environmental factors can also be used to improve tactile, proprioceptive and vestibular senses, adaptive motor responses. Toys in different textures, ropes, hula hoops, vibration toys, pillows, ramps, swings, mats, scooter boards are used to stimulate the sensory system. It is aimed to increase the motivation of the child, to ensure his active participation, and especially the sensory part of the motor control process is supported.

Family-Centered Approaches
The 4 basic principles of family-centered approaches are as follows:
– It does not try to normalize development, instead it focuses directly on functional tasks and supports functional performance.
– It defines the periods of change, and the families are the ones who best define that the child is trying to do a new task.
– Defines the environment and the task.
-Encourages practice, ensures repetition of movement in different environments.

Coping With and Caring for Infants with Special Needs (COPCA) COPCA program is a family-centered early rehabilitation program applied to risky babies.
It is a method organized by the physiotherapist and applied by the family according to the child’s abilities and environment. The aim of this program is for the family to overcome the child’s problem using their own capacity. For this, the family needs a special trainer (coach). The special trainer (physiotherapist) does not tell the family what they can or should do, but helps the family discover the practices that can be done. The physiotherapist listens to the family, observes, makes suggestions and informs and supports them. The family, with the help of the physiotherapist, takes the main responsibility in deciding on the care and treatment of the child.
Family Oriented Support Training Based on Home Program is one of the most important parts offamily education and home program rehabilitation practices. Early rehabilitation includes not only the baby but also the family. Families should be trained on the positions, approaches and behaviors they will apply during the day. Positioning and holding techniques should be adapted to daily activities and home environment. Families should be ensured to understand the objective of the proposed positions and activities. Families should apply movements in daily life without passivating the child in functional activities, and necessary information should be provided on this subject.

Target-Oriented Treatment
Target-oriented treatment method is a method that facilitates the child’s participation in daily activities and adaptation to various situations in life in children with developmental disorders. Treatment goals are selected based on close cooperation between the family and the versatile professional rehabilitation team. The objectives set should be specific, measurable, achievable, fit for purpose and well-timed (SMART). In the targeted treatment method, the treatment is organized for the purpose and allows the inclusion of motor learning principles based on the existing theories about motor development. Setting goals by grading allows individual evaluation of treatment outcomes. The results are evaluated with Goal Attainment Scale (GAS).

Leave a Reply