Sucking, chewing, swallowing and saliva problems are rarely encountered during childhood from the newborn period. Regardless of the reason, starting early diagnosis and treatment as soon as possible will help to reduce serious problems such as nutritional deficiency, growth retardation, aspiration, and lung infections. Ingestion is a dynamic event that requires harmonious functioning of the lips, tongue, palate, pharynx, larynx and esophagus muscles. The maturation of the oral and oesophageal structures and the evolution of the absorption process are parallel to the development of the brain and nervous system. Anatomical abnormalities in any of these elements, impaired effectiveness, duration and timing of swallowing may cause saliva and food to escape into the respiratory tract. It is estimated that approximately 1% of childrenin the community have swallowing difficulties. This rate is higher in children with cerebral palsy, traumatic brain injury, neuromuscular diseases, craniofacial structural disorders, congenital heart diseases, airway anatomical disorders, and early birth history. Infants and children also experience swallowing disorders due to behavioral, developmental, or neurological disorders, respiratory issues, and structural changes such as gastroesophageal reflux (GER), cleft lip, or hard palate. Fatal aspiration pneumonia has been described, especially in the neonatal period. It has been shown that neonatal aspiration syndromes occur in 4% of all live births and are highly associated with morbidity and death.
ANATOMY OF SWALLOWING
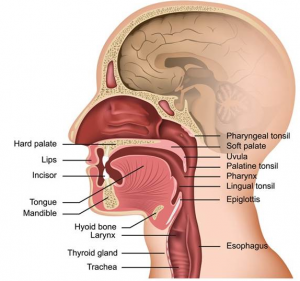
Foods follow an anatomical route starting from the oral cavity to the pharynx, larynx, hypopharynx, esophagus and from there to the stomach. Before starting this anatomical pathway, it also sees the lips, teeth, tongue, cheeks, oral vestibular, palate and palatal arcs in the mouth.
Lips take the shape of mouths. M. orbicularis consists of oris and submucosa. They are covered with skin from the outside and mucous membrane from the inside. Contraction of M. orbicularis oris narrows the mouth and closes the lips like a sphincter. That’s how he keeps the bolus in his mouth.
Cheeks are a structure that forms the side walls of the oral cavity and is integrated with the lips. M. buccinator consists of parotid canal, buccal and molar glands, veins, nerves, lymphatics, fat and mucosa. M. buccinator fibers and m. orbicularis oris fibers support each other. The parotid canal punctures the M. buccinator before opening into the oral cavity opposite the second upper molar tooth. During chewing, it contracts and presses the cheeks to the teeth and stretches the cheeks to prevent food accumulation between the teeth and cheeks.
It separates thehard palate, mouth and nose cavities. The anterior part consists of maxillary and the posterior part consists of palatine bones.
The posterior part provides an attachment area to the soft palate. The alveolar arch is located in front of and next to the mouth surface of the hard palate.
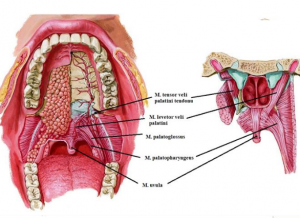
The soft palate separates the nasopharynx from the oropharynx. It is covered with mucosa and consists of palatine aponeurosis (m. tensor parent palatine tendon), taste buds, mucous glands and muscles. The high soft palate closes the pharyngeal ischemia during swallowing. This separates the nasopharynx from the oropharynx and thus prevents nasal insufficiency. Soft palate depression closes the oropharyngeal isthmus.
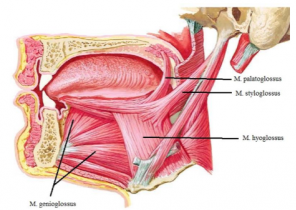
Thetongue is attached to the mandible by m. genioglossus, to the hyoid bone by m. hyoglossus, to the processus styloideus by m. styloglossus, to the palatine bone by m. palatoglossus.
These four muscles make up the eccentric muscles of the tongue. They take the origin of the tongue from the outside and end up in the tongue.
- Genioglossus is in the form of a fan at the bottom of the tongue. The back fibers pull out the tongue. The front fibers pull in the tongue. If each section works together, it pushes the tongue down. In this way, a front-to-back groove is formed on the tongue and functions during the suction function.
- Hyoglossus goes up vertically from the hyoid bone. It convexizes the back of the tongue by pulling down the edges of the tongue.
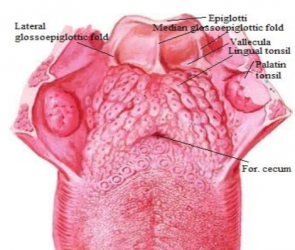
- Styloglossus pulls up the edges ofthe tongue to form a pit for swallowing and they also help to retract the tongue.M. palatoglossus is actually the soft palate muscle. The muscles of both sides begin as a continuation of each other from the front of the soft palate. It ends on the back of the tongue by attaching to the tongue from the side. It pulls the tongue up, closes the oropharyngeal isthmus, and helps to start swallowing. This muscle also protects the palatoglossal arch, preventing the saliva from spilling from the vestibule to the oropharynx. The insentric muscles of the tongue are m. longitudinalis superior, m. longitudinalis inferior, m. transversus linguae and m. verticalis linguae .Their main task is to change the shape of the tongue.
- Longitudinalis Superior curves the tip and edges of the tongue, making the tongue concave.
- Longitudinalis Convexizes the upper part of the tongue by folding down the inferior tip of the tongue.
- Transversus linguae lengthens your tongue narrowly.
- Verticalis linguae turns the tongue surface into a wide plateau. By working together, they perform fine movements during speech, chewing and swallowing.Teeth play an important role in chewing.
Tooth loss causes loss of alveolar arches. Teeth and alveolar regions are surrounded by gums (gingivae). Teeth begin at the 6th month and continue to grow until the age of 2. The replacement of deciduous teeth with permanent teeth starts at about 6 years of age and continues until adulthood. As the permanent teeth begin to come in, the maxilla and mandible extend forward to make room for them.
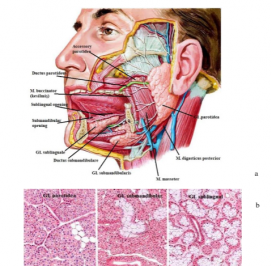
The minor and major salivary glands secrete saliva into the oral cavity. The minor glands located in the submucosal and mucosal layer of the tongue and cheeks secrete mucus directly or through small ducts into the oral cavity.
The major glandular glands are the glandula (gl.) parotidea, gl. submandibularis and gl. the sublingualis are glands .
Gl.the parotidea is located on the side of the face partially in front of and below the external auditory canal. It is the largest of the salivary glands. It consists entirely of the serous layer .
Gl. The submandibularis consists partly of mucous tissue and densely of the serous layer.
Gl. The sublingualis is the smallest salivary gland. It consists entirely of a mucous layer.
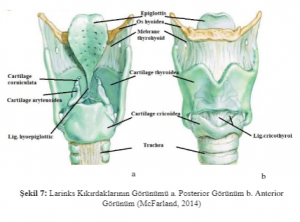
The larynx consists of a cartilage structure held together by muscles and ligaments. The laryngeal space is continuous with the pharynx at the top and the trachea at the bottom. It is located at C3-C6 level. The formation of the sound is provided here. It acts as a sphincter that prevents foreign bodies from escaping into the respiratory tract. The larynx acts in conjunction with the os hyoideum. It is provided by the supra-hyoid muscles that attach to the os hyoideum, allowing it to move forward and upward during swallowing. It can also be displaced according to the position
of the head.Cartilago epiglottica prevents aspiration by closing the trachea during swallowing.
The pharynx is a semi-cylinder structure attached to the skull base above, continuing with the esophagus at the C6 level below. The anterior pharyngeal walls are associated with oral cavity, nasal cavity and larynx. The pharynx cavity forms a common pathway for air and nutrients. Nasopharynx is the uppermost part of the pharynx. This section behind the nasal cavity is located at the level of the base of the head frame and the posterior edge of the soft palate. It is related to respiratory and auditory organs. The cartilage of the eustachian tube swells by pushing the pharynx mucosa. This bulge is more pronounced in the back. This bulge forms the m. levator veli palatini and the torus tubarius together with the upper mucosa. Mucosal folds in the nasopharynx cover the salpingopharyngeus (salpingopharyngeal fold) and m. levator veli palatini. These two muscles open the cartilage end of the eustachian tube by pulling in opposite directions during swallowing. In this way, the pressure balance between the middle ear and the nasopharynx is achieved.
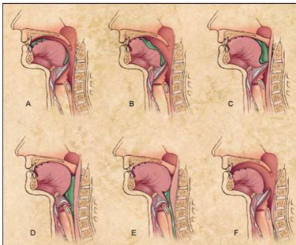
How is the Swallowing Process Performed?
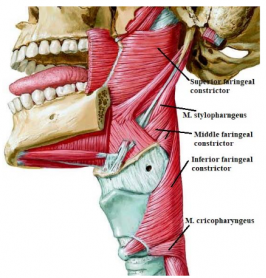
During swallowing, the soft palate expands in all directions by pulling upwards and the bite in the mouth passes to the pharynx. As a result of contractions of M. stylopharyngeus, the side walls of the pharynx are pulled up and towards the laterals. Thus, the diameter of the pharynx in the transverse direction expands. As the larynx and tongue move forward, theanteroposterior diameter expands. As soon as the food enters the pharynx, the muscles that lift the pharynx relax and the pharynx goes down. The superior part of the external muscles bulges the upper edge toward the anterior side of the pharynx mucosa. This blister is called a Pasavan blister. The soft palate is also pulled backwards and upwards to reach the Pasavan bulge. Thus, the upper and middle parts of the pharynx are disconnected. Meanwhile, the constrictor muscles of the pharynx start from the top and contract downwards and allow the bite to progress to the esophagus. The food is prevented from escaping upwards. These muscles are innervated by the plexus pharngeus nerve from the n. vagus.
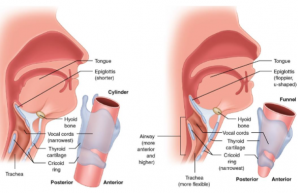
Developmental Anatomy
There are serious anatomical differences betweenadults and infants.Infants don’t have teeth. The hard palate is flatter than adults. Hyoid bone and larynx are located at a high level. The larynx opens directly to the nasopharynx. Epiglottis is in contact with the soft palate at the back. With the transition to adulthood, the cervical vertebra and soft tissue length increase and the larynx and hyoid bone shift downwards. The soft palate contact of Epiglottus disappears. These changes support speech development. However, it increases the likelihood of exposure to nutrient aspiration.
THE PROCESS OF SWALLOWING
Nutrients, which are the source of human nutrition, pass through the swallowing function to the digestive system. The swallowing process is a partially voluntary controlled process. In other words, it initiates and maintains the swallowing function with human will. But swallowing also involves involuntary, reflexive processes. The act of swallowing can be considered as 3 phases in some sources and 4 phases in some sources. These are;
- oral preparation,
- oral
- pharyngeal and
- are esophageal phases.
The oral preparation phase involves taking the food into the mouth, turning it into a bolus (bite) and preparing it for swallowing. This entire phase is carried out voluntarily. At this stage, other structures (pharynx, larynx) are in resting position.
Theoral phase, like thepreparatory phase, is voluntary and carries out the pushing of the nutrient into the bolus and towards the pharynx. The transit time through the mouth is 1-1.5 seconds. Palatal and lateral swallowing reflexes are triggered as the bolus reaches the anterior plicae and the pharyngeal phase begins.
Unlike the oralphase, the pharyngealphase is involuntary, a process that occurs with rapid and reflexes. This phase occurs by lifting the soft palate to protect the airway, moving the larynx forward and upward; closing some cartilage structures and vocal cords. The transition time of the pharyngeal phase is one second. As the bolus passes through the cricopharyngeal region, the esophageal phase of swallowing begins.
In the esophageal phase, the bolus reaches up to the stomach. The esophageal stage begins with the relaxation of the upper esophageal sphincter, followed by esophageal peristalsis. As the bolus passes through the lower esophageal sphincter at the junction of the stomach and esophagus, the food taken from the mouth is delivered to the stomach. The transition of the bolus to the stomach takes place symmetrically. Esophageal transition time varies between 8-20 seconds depending on the bolus consistency.
Swallowing disorder (Dysphagia)
Occurs as a result of physiological changes in the muscles required for swallowing. Physiological changes cause two types of swallowing disorders:
1) Disorders related to the preparation of the bolus to ensure the passage of the bolus from the mouth to the stomach
2) An attempt to swallow the material for the passage to the pharynx and esophagus as a result of misdirection of the bolus ready for the passage is only a failure to reach the stomach.Swallowing disorder is not a disease. However, it can occur asa result of many conditions or diseases such as stroke, head and neck cancers, head trauma, progressive neurological diseases, old age, developmental deficiencies, prematurity, and can be a symptom of many diseases.
- Malnutrition, dehydration, persistent cough or aspiration pneumonia may occur.
- In the oral phase, deterioration in lip closure may cause food to fall from the mouth.
- The anomaly of the facial muscles can cause food to remain in the outer oral cavity.
- Disruption of the floor muscles of the mouth may cause the food to accumulate and remain in the floor of the mouth after swallowing.
- Impairment of tongue movements causes loss of effective chewing, food cannot be bolus and food cannot be emptied out of the oral cavity.
- If the patient can’t drag the bolus back, there’s residue on the palate.
- If the velopharyngeal closure in the soft palate deteriorates, it may cause food to enter the nose during swallowing.
Neural Control of Swallowing
Brainstem (Bulbar) Swallowing Center
There are two centers in the bulbar region related to swallowing. These are located in the nucleus ambiguus, in the ventral of the bulbus, and in the dorsal of the nucleus tractus solitarus. These two nuclei are located bilaterally and symmetrically. Neurons that organize the motor network of swallowing function are premotor neurons or inter neurons. This neuronal network system appears as “Central Pattern Generator” (CPG). Even if a single bite is swallowed, the necessary muscle contraction and relaxation sequence and synergistic adaptation are provided by the CPG in the brainstem . It is classified into three levels that constitute the CPG network in the brainstem of theswallowing function:
a) Afferent part: The sensory level that reaches the neurons that make up the CPGs where cortical and subcortical descending signals are accepted with
sensory inputs from the periphery.
b) Efferent part:The motor level at which the motor nuclei of the relevant cranial nerves perform the contraction order to the swallowing
muscles in the motor neuron pool in coordination.
c) Interneural network part:The level consisting of premotor neurons that organize the swallowing to be performed in a longitudinal and bilateral manner between the afferent and efferent levels.
Cortical Swallowing Center
An adult person also voluntarily initiates swallowing of the cortex.
So the cortex would activate the CPG network in the bulbar region. On the other hand, it was determined that swallowing function started in the human fetus after the 12th gestational week. This shows that swallowing can only be performed with the brain stem. Although our knowledge of the cortical regions associated with ingestion has increased significantly through functional magnetic resonance imaging studies, the exact central control mechanism for ingestion is still not fully understood. In studies using brain imaging techniques such as functional magnetic resonance imaging and magnetoencephalography, which are among the special examinations, cortical regions activated during swallowing were investigated. Tongue rounding, chin tightening, lip joining movements, which are oral movements, have been reported to be the most active cortical parts of the prefrontal cortex, sensorimotor cortex, anterior part of the gyrus cinguli, insular cortex
and parieto-temporal cortex. Studies usingspecial imaging methods have shown that cortical swallowing areas are asymmetrical, bilateral and multipartite. It has been determined that swallowing is localized in the insular cortex region deep in the frontal, parietal and temporal opercular regions of the right hemisphere, especially in people with dominant right hand. Some researchers have stated that there is a functional predominance in swallowing or a time-dependent shift of cortical activation from left to right to the sensorimotor cortex during voluntary swallowing.In
summary, voluntary and reflexive swallowing is controlled by widely distributed bilateral and multifocal cortical networks, including overlapping cortical regions.
Evaluation Methods in Pediatric Difficulty of Swallowing
Evaluation of swallowing difficulty inpediatric dysphagia patients is generally classified as the patient’s anamnesis, bedside clinical evaluation and instrumental evaluation.The reliability of anamnesis alone or bedside clinical evaluation methods is quite low. Questioning prenatal, birth and newborn history can give important clues in determining the etiology of nutritional and swallowing problems in children. For this reason, a multi-faceted perspective is necessary in the evaluation of pediatric dysphagia.
Clinical Evaluation
In clinical evaluation, whether the child has anatomical, neurological, behavioral, respiratory or connective tissue problems is evaluated.
Evaluation of Behavior, Condition and Sense Integrity
The child’s state of alertness before, during and after nutrition, signs of stress during or after nutrition, and the child’s reactivity to sensory stimuli should be recorded. Symptoms such as sudden contractions, shortness of breath or acceleration, sweating, and silent crying that develop in the body and extremities of the child during or after the feeding period should be seen as symptoms of stress. The problem of food rejection may be physiologically based due to respiratory distress or gastrointestinal cause, or it may also be due to oral sensorimotor deficit or problematic parental interaction with the child. During feeding, the head should be turned to one side, deliberate vomiting, spitting should be questioned and noted.
Tonus and Postural Control
Evaluation head, neck and trunk control is necessary for successful nutritional activity. Muscle tone should be recorded by evaluating abnormal movement patterns and compensatory behavior models, if any. In a healthy child, independent sitting and head control should be provided at the 5th-7th months of motor development. For this reason, postural evaluation should be performed according to motor development steps.
Assessment of Respiratory Condition
There is a close relationship between swallowing and respiration.The fact that the neural control centers in the brainstem (CPG) of swallowing and respiratory functions are very close to each other, and that they use similar neural pathways and common oropharyngeal structures necessitate a highly developed coordination between them. In pathological cases, this coordination may be impaired. For this reason, respiration is very important in clinical evaluation. Respiratory changes should be observed before, during and after feeding. Respiratory type, frequency and depth should be noted and it should be checked whether they are among the normal values suitable for the patient’s age.
Weight Gain Evaluation
Slowing or stopping the child’s weight gain in the last 2-3 months is important and may support swallowing difficulty along with other evaluation parameters. Regular and appropriate weight gain, especially in the first 2 years of life, is important for brain and body development.
Physical Evaluation of Oromotor and Laryngeal Regions
Tonus is evaluated by examining the neck area with palpation. Contraction in the neck muscles affects the elevation of the hyoid bone. Hyoid bone, which is not sufficiently elevated, disrupts laryngeal mobility and the kinesiology of the Upper Esophageal Sphincter (UES). When the jaw is slightly open in the resting position, the presence of asymmetry and the side with slippage are recorded. The adequacy of lip closure, the presence of asymmetry in the tongue, and the mobility of the tongue inside and outside the mouth should be evaluated. If there is an abnormal movement pattern in the oral region, such as the tongue repulsion reflex, it should be recorded. The dental version appropriate for the age of the child should be evaluated. Delayed tooth development affects chewing and swallowing function. Gag reflex should be tested with the help of Abeslang. Unilateral palate movement suggests unilateral bulbar damage. Intraoral secretion or saliva evaluation is performed and the prediction about the phase of swallowing may be insufficient is obtained by paying attention to the region where the saliva accumulates.
Scale Evaluation
There are various non-standardized scales used in the clinic for the evaluation of swallowing and nutritional status in children. In these scales, the target population, age range, evaluation method, and scoring system vary. These scales used in the clinic also determine the need for instrumental evaluation methods of the patient. The 90 mL water swallowing test, which has high sensitivity in terms of determining the risk of aspiration inclinical evaluation, is one of the frequently used scales. During the evaluation, the child is given 90 mL of water and asked to drink continuously. The occurrence of hesitation during drinking water, coughing during or immediately after drinking water, change in sound quality, presence of wet sound, abnormal swallowing are considered.
As an example of scales used in healthy children;
Summary Assessment of Motor Function (Oral Motor Deviation scale) (BAMF-OMD),
Children’s Eating Behavior Inventory (CEBI, 1991)22 and
Schedule for Oral Motor Assessment (SOMA),
Feeding Questionnaire, Neonatal Oral-Motor Assessment Scale (NOMAS, 1985) used in preterm infants,
Feeding and swallowing Questionnaire, Oral Motor Assessment Scale (OMAS, 2009) used in children with cerebral palsy,
Used in children with autism spectrum disorder; Eating profile,
It is used in children with chronic diseases; About Your Child’s Eating (AYCE, 2007)
Instrumental Assessment
There are various devices that are used for instrumental assessment of swallowing disorder in children with dysphagic SP. Among these devices; Videofluoroscopic Swallowing Study (VFIC), Fiberoptic Endoscopic Evaluation of swallowing (FEEDS) and ultrasound allow visual evaluation of the oral, pharyngeal and upper esophageal phases during the phases of swallowing.
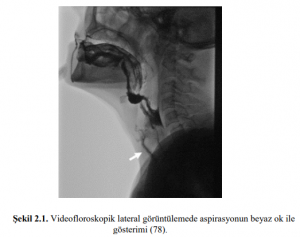
Videofluoroscopic Study of Swallowing
The Videofluoroscopic Swallowing Study (VFIC) is also known as the Modified Barium Swallowing Study. It is considered the gold standard in the evaluation of swallowing mechanisms. 18 First of all, this evaluation is made to patients who are deemed appropriate in clinical evaluations. Patients diagnosed with difficulty swallowing are placed on a suitable chair and tested by giving nutrients mixed with radiopaque substances. At the end of the test, a dynamic assessment of the oral preparation, oral, pharyngeal and esophageal phases of swallowing is provided. If necessary, different consistency, postural changes and swallowing maneuvers are included in the test protocol. The test begins with a minimal dose and gradually the dose is increased. The moment of swallowing is assessed by monitoring it on the monitor using images of the lateral and frontal planes. This test is tongue and the timing of movement, part oral pozisyonal you change, you’re epiglotis kinematics, laryngeal elevation, UOS narrowing of the esophagus to the stomach allows for the assessment of progress and swallow you whole. At the end of the test, an opinion is given on the degree of aspiration or penetration. The use of contrast media, partial exposure to radiation, the fact that the test gives only a two-dimensional image, and the high cost are listed as the most important disadvantages of the videofluoroscopic swallowing test high cost.
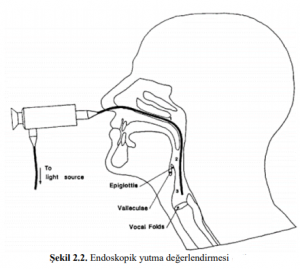
Endoscopic Evaluation (FEES)
Fiberoptic Endoscopic Evaluation (FEEDS) developed by Langmore is a frequently used evaluation method by researchers.It is entered through the nose with a fiberoptic laryngoscope and provides information about the anatomy of the swallowing pathways and the residue of the stained bolus and the risk of aspiration. It measures the response of pharyngeal and laryngeal structures to the stimulus. According to VFSS , it provides a closer view of the laryngeal vestibule, vocal cords and upper trachea, but the fact that swallowing cannot be seen, does not show the relationship between oral, pharyngeal and esophageal structures, the inability to monitor swallowing physiology completely, is an interventional approach and requires cooperation are the most important disadvantages of this method.
Submental EMG Method (SB-EMG)
Electromyography (EMG) records and analyzes the electrical signals generated in the specified muscle and provides information about the innervation and electrical potential of that muscle. EMG method is divided into 2 types as needle method in which nerve conduction using needle electrodes is examined and superficial EMG (y-EMG) method in which superficial electrodes are used.

Ultrasound is rarely preferred overother instrumental evaluation methods. It provides information about the direction of movement and activation of the relevant muscle during swallowing. In particular, it provides the opportunity to evaluate the pharyngeal phase muscles quantitatively and in
real time.
Treatment Approaches in Pediatric Difficulty of Swallowing
Treatment methods used in pediatric swallowing disorders are shaped by many sub-parameters such as the current diagnosis of the child, general physical capacity, perception status, nutritional strategy and the pathophysiology of swallowing disorder. Detailed history, clinical and instrumental evaluations play a key role in establishing the treatment procedure.
The main purpose of treatment in swallowing difficulties is to prevent lung infection that causes an increase in morbidity and mortality, to prevent malnutrition and dehydration, and to increase the quality of life by maximizing the current diet. In the treatment of swallowing difficulties, the target should be determined in the light of all these parameters. Traditional dysphagia rehabilitationin
children includes diet, nutrition, strengthening exercises of oropharyngeal muscles, posture and environmental modifications, swallowing maneuvers and special motion-based techniques, pressure stimulation to increase thermal, tactile and sensory input.
Oropharyngeal Exercises
Orophageal exercises are included in the treatment of swallowing disorder in the form of active, passive and sensory approaches. Exercises involving range of motion created by the child’s own muscle strength are active exercises. Examples of these exercises are tongue strengthening exercises, the aim of this treatment step is to increase muscle strength and endurance. Exercises should be specific to each child. Massage and stretching exercises are also included in passive oropharyngeal exercisesin children. Increasing circulation, providing motor learning, reducing abnormal oral reflexes, regulating muscle tone are listed as the benefits of passive oropharyngeal exercises in dysphagic patients. Sensory approaches generally consist of applying heat, cold, electrical stimulation, high-frequency vibration, or other activities that involve stimulation of the skin and muscle tissues. Increasing oral awareness enables reduction of excessive gag reflex and support of motor learning.
Neuromuscular Electrical Stimulation
Neuromuscular electrical stimulation (NMES) is a method known to be included in swallowing rehabilitation in 2006, when it was first aimed to stimulate deep muscles by placing an electrode in the anterior neck.In this method, the hypothesis is that electrical stimuli will increase pharyngeal muscle strength with accelerated cortical rearrangement. NMES, which is most commonly used in swallowing rehabilitation in the clinic, is an application with a frequency of 80 Hertz, a transition time of 300-400 microseconds and its trade name is Vital Stim.

Sensory Stimulation
Sensory stimulation approaches are one of the most commonly used methods in the treatment of swallowing disorders. It usually aims to improve intraoral awareness and prevent delay in swallowing reflex. One of the more recent approaches to assessing pharyngeal sensory integrity and eliciting swallowing is the air spray technique. Studies by blowing air during flexible endoscopy report that the pharyngeal sensation decreases with age.Thermal tactile stimulation is the most commonly used sensory stimulation method in dysphagic patients with delayed swallowing reflexes. Thermal tactile stimulation method is an approach that includes cold and slight touch sensation to the anterior pharyngeal arches in the oral cavity.

Postural Techniques
Some special postural techniques that require cooperation in children can compensate for swallowing pathophysiology in some cases. These techniques do not correct motor impairment and pathophysiology, but only temporarily compensate for the process. In the case of insufficiency in the oral transfer of the intraoral bolus, there are special postural techniques such as head extension; 45° flexion of the head in the case of delayed swallowing reflex or vallecular residue (jaw down position), head rotation to the damaged side in unilateral laryngeal dysfunction, and flexion of the head to the intact side in decreased pharyngeal contraction. However, it is appropriate to determine the appropriate postural technique after making sure that it prevents aspiration in the videofluoroscopic swallowing study before teaching the patient.
Postural Maneuvers
Postural maneuvers to be performed in children withcooperation are compensation mechanisms that ensure that the bolus is delivered to the esophagus in the most effective and safe way, just like postural techniques.Before placing postural maneuvers in the treatment protocol, it is necessary to test them in the VFYÇ assessment method, if possible. The purpose of these maneuvers is to adjust the pressure applied on the nutrient by changing the flow direction and speed of the nutrient. In the forceful swallowing technique, it is aimed to apply strong pressure on the food during swallowing, thus increasing the contact between the tongue root and the pharyngeal wall and preventing the delay in the swallowing reflex. There are also special manoeuvres in the Supraglottic Swallowing Maneuver, such as the Super-Supraglottic Swallowing Maneuver and the Mendelson Maneuver. However, full compliance is essential for the use of these special approaches in pediatric patients.

Leave a Reply